Some people might avoid talking about it, but like it or not, we can’t ignore vaginal dryness. Vaginal dryness is a common experience for menopausal women, but that doesn’t mean you have to accept it.
Let’s discuss the details of this uncomfortable symptom: what it feels like, what causes it, and the many treatment options available to relieve it.
Understanding menopausal vaginal dryness
Vaginal dryness is a common problem during peri- and post-menopause. It’s the primary symptom of the genitourinary syndrome of menopause (GSM)—previously called vulvovaginal atrophy— and it affects over half of all menopausal people.
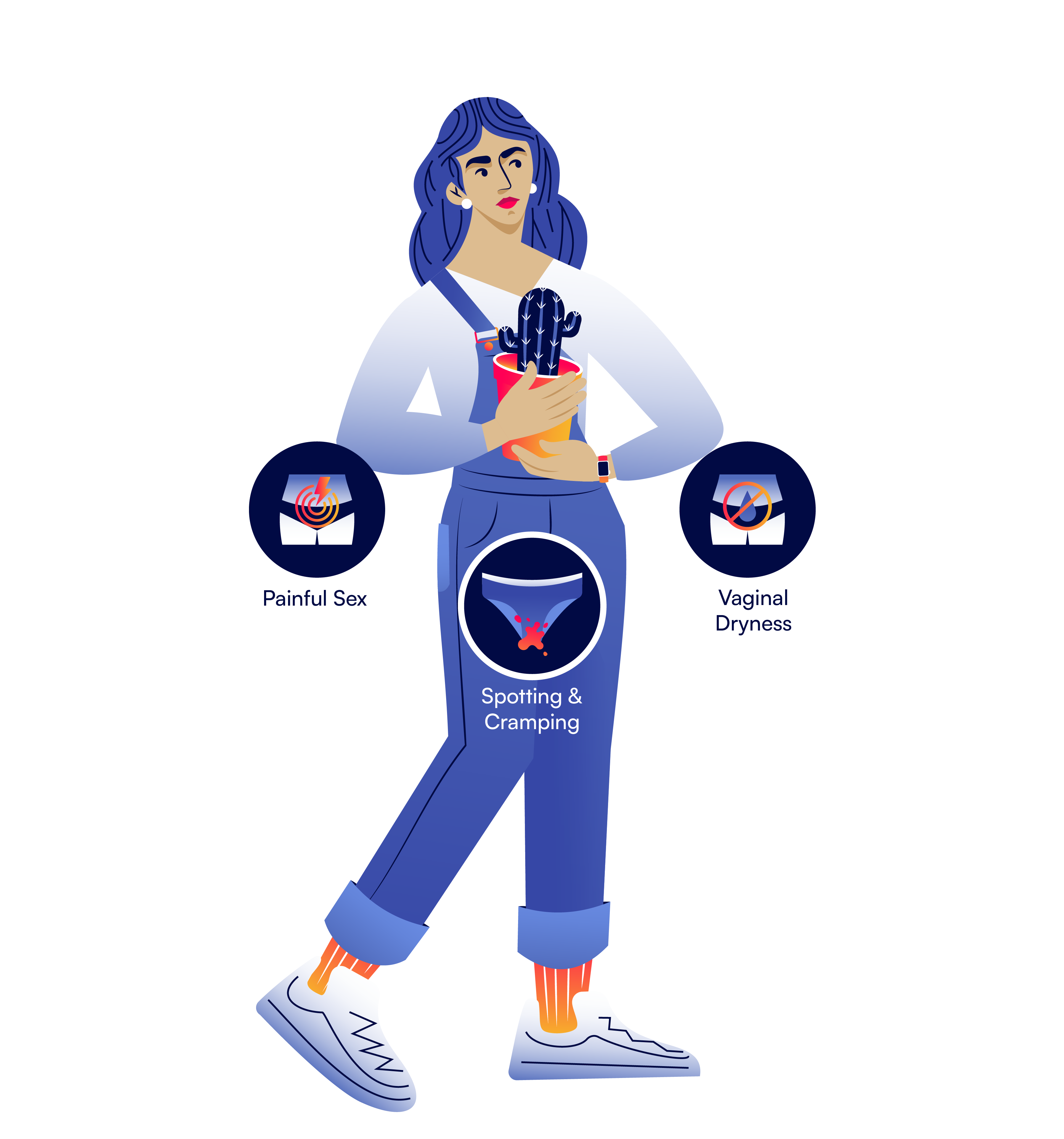
GSM symptoms are wide-ranging and can seriously impact your quality of life. These symptoms include:
Dryness, itching, burning, or irritation of the vagina and/or vulva
Sexual dysfunction, including discomfort, low desire or arousal, and reduced satisfaction
Painful intercourse, called dyspareunia
Bladder symptoms, including painful urination, urinary urgency, or recurring urinary tract infections (UTIs)
What vaginal dryness looks (and feels) like
As you progress through menopause, you may notice some uncomfortable physical changes due to GSM.
Your labia and vulva might lose fullness, your vaginal canal opening might become more narrow, and your vaginal lining might feel irritated and inflamed. Elasticity and pliability decrease with a lack of estrogen.
Because your vaginal walls are more fragile, you may experience bleeding after intercourse. Whether you experience one symptom or several, they can make sex uncomfortable and impact intimacy.
The most common urogenital symptoms of menopause by percentage are:
27%: vaginal dryness
18%: vaginal itching or irritation
11%: vaginal discharge
GSM symptoms get worse as you age and usually require treatment to improve. There’s no reason to suffer in silence: talk with your provider to find treatment and relief.
What causes vaginal dryness?
Before menopause, your body’s high estrogen levels stimulate blood flow to the genital region, vaginal tissue growth, and glycogen production. Glycogen then feeds the “good” bacteria, called lactobacilli, that help keep the vagina healthy, acidic, and infection-free.
As estrogen levels fall during menopause, your vaginal microenvironment changes significantly. The number of “good” lactobacilli bacteria decreases, vaginal pH becomes less acidic, and the quality and quantity of vaginal discharge shift.
Low estrogen also causes several physical changes in the vagina, including:
Loss of vaginal elasticity
Thinner, more fragile vaginal tissue
Shortening and narrowing of the vagina
When vaginal dryness disrupts your life
When vaginal dryness occurs, it often brings bigger problems along with it. One survey of over 3,000 menopausal women with GSM symptoms found that:
59% said GSM symptoms decreased their enjoyment of sex
23% said GSM symptoms negatively affected their enjoyment of life
Another study of 1,000 heterosexual couples showed that menopause-related vaginal discomfort profoundly affected their intimate relationships.
58% of women said they avoided intimacy because of discomfort. 78% of male partners believed vaginal dryness was the reason their female partners were avoiding intimacy.
Vaginal dryness can certainly cause physical pain, but it can also cause emotional pain. If you’re dealing with uncomfortable GSM symptoms, know that you’re not alone and treatment options exist.
How to relieve, treat, and reverse vaginal dryness
Vaginal dryness in menopause is to be expected, but it doesn’t have to be endured. Numerous treatment options exist to relieve your symptoms and improve your quality of life. Talk with your healthcare provider to determine which treatment options best suit your needs.
Available treatments to relieve vaginal symptoms, including dryness, include:
Over-the-counter and non-hormonal: Moisturizers and lubricants
Prescription and hormonal: Vaginal estrogen and DHEA
Non-FDA-approved alternatives: CO2 laser treatment
Vaginal moisturizers
Vaginal moisturizers are non-hormonal topical creams or gels that help reduce discomfort and irritation. Similar to lotions you use on your skin, these moisturizers rehydrate your vaginal tissue by absorbing into the lining of the vagina.
Vaginal moisturizers offer long-lasting hydration by supporting your natural pH level and mimicking healthy vaginal fluids. Relief typically lasts 2-3 days, but consistency is key! The more severe your symptoms, the more frequently you’ll need to use a moisturizer.
The quality of vaginal moisturizers varies greatly, and some contain irritating ingredients. When choosing a moisturizer, look for one that:
Has a pH between 3 and 5, the vagina’s “happy” pH ranges
Is paraben-free, as parabens may cause serious adverse effects
Is hyaluronic acid-based, which can help rebalance vaginal hydration
Vaginal lubricants
Lubricants are another over-the-counter, non-hormonal option to help relieve vaginal dryness. They can be water-, silicone-, or oil-based. Water-based lubricants won’t stain and may be better for sensitive skin, while silicone-based formulas last longer.
Lubricants are particularly useful if your dryness causes pain and discomfort during sex. You can apply lubricants to the vagina and vulva, as well as a toy or your partner’s penis, before sexual activity. This helps reduce friction and increase comfort during penetrative sex.
A lubricant’s benefits last while it remains on your skin, but not any longer. Reapplying lubrication during sex can help avoid friction and discomfort. Like moisturizers, many lubricants contain ingredients that irritate the skin. Look for one that:
Has an osmolality between 200–600 mOsmol/kg, as lower osmolality reduces the risk of vaginal irritation
Has a pH between 3 and 5
Is paraben-free
Vaginal estrogen
If moisturizers and lubricants don’t resolve your vaginal dryness, vaginal estrogen is the recommended prescription treatment.
Vaginal estrogen is a form of hormone therapy (previously called hormone replacement therapy) that can improve your symptoms within a few weeks of starting treatment. This option helps relieve vaginal symptoms and reduces your risk of urinary tract infections.
Vaginal estrogen is typically low-dose, and you use it locally by inserting the cream, capsule, or ring directly into your vagina.
Because you use it vaginally, most of this estrogen stays in the vagina and minimally affects the rest of your body. Vaginal estrogen doesn’t increase your risk of endometrial cancer, and there is no evidence linking it to breast cancer.
Several FDA-approved vaginal estrogen options are available to treat vaginal dryness, including:
Cream: Provides a moisturizing effect, but can be messy
Dissolving tablet: Offers more controlled dosing and less mess than cream
Vaginal ring: Can be low-dose for vaginal symptoms or higher-dose for widespread menopausal symptoms
Softgel capsule: Reduces systemic estrogen absorption when compared to a vaginal tablet
Vaginal DHEA
Vaginal dehydroepiandrosterone (DHEA) is a hormone therapy that works by converting into estrogen once it’s inside your body. Vaginal DHEA may be an alternative for those who aren’t candidates for vaginal estrogen.
This daily medication has been shown to improve:
GSM symptoms, including painful sex
Vaginal pH, which helps fight against infection
Vaginal atrophy, which causes dryness and irritation
Alternative options
Small, uncontrolled trials have tested carbon dioxide (CO2) laser treatments to help with GSM symptoms such as vaginal dryness. These trials found positive results, but there’s not enough evidence to support using laser treatments for GSM.
Laser treatments can be expensive, and they’re not FDA-approved or supported by the Menopause Society.
Your healthcare provider may consider suggesting these experimental procedures if you are unable to use hormone therapy or prefer a non-FDA-approved option.
Stop vaginal dryness in its tracks with tracking
Some menopausal symptoms, such as hot flashes, gradually improve on their own. However, the genitourinary syndrome of menopause only gets worse over time if left untreated.
Remember: GSM symptoms aren’t limited to vaginal irritation during sex: dryness, discomfort, and UTIs can affect you regardless of your sexual activity status.
Tracking your symptoms empowers you to prevent this worsening. It helps you understand the type and extent of your symptoms so you feel ready to talk with your healthcare provider.
The knowledge that tracking provides gives you the power to get the care you need. With details about your symptoms, your provider can better determine which treatment will bring you relief.
Questions to ask your provider
Talking with your healthcare provider about GSM symptoms might feel a bit uncomfortable at first. After all, symptoms like vaginal dryness, recurrent UTIs, and painful sex are personal, and unfortunately, they still carry some societal stigma.
However, you’re not the first to ask, and you certainly won’t be the last! Here are a few questions to get your conversation started:
I’ve been using my smartwatch to track the progression of my vaginal symptoms, mainly vaginal dryness. Can I get your opinion on my symptoms and what my treatment options are?
I’m experiencing vaginal dryness that’s interfering with my daily life and my relationship with my partner. Do you think hormone therapy would help relieve my symptoms, or should I pursue a non-hormonal option?
DISCLAIMER
This article is intended for educational purposes only, using publicly available information. It is not medical advice, and it should not be used for the diagnosis, treatment, or prevention of disease. Please consult your licensed medical provider regarding health questions or concerns.
Want support through the transition?
Sign up for early access to Amissa and stay informed as we grow.
